 Gastric sleeve surgery, also called sleeve gastrectomy, is in the category known as restrictive bariatric surgery. Because it doesn’t interfere with absorption, it is appropriate for people with anemia or Crohn’s disease or other conditions where gastric bypass is not a good choice. As with the other procedures, the patient goes through extensive physical and psychological screening.
Gastric sleeve surgery, also called sleeve gastrectomy, is in the category known as restrictive bariatric surgery. Because it doesn’t interfere with absorption, it is appropriate for people with anemia or Crohn’s disease or other conditions where gastric bypass is not a good choice. As with the other procedures, the patient goes through extensive physical and psychological screening.
Sleeve gastrectomy may be especially appropriate for two kinds of patients: those of advanced age and those in remote areas. Those of advanced age are relatively safer, because they will not necessarily be alive to suffer from any presently unknown long-term effects. Also, people who live in remote areas with poor transportation benefit from this type of surgery, because it does not require as much follow-up care as other varieties.
Because it is irreversible, this option is a genuine commitment. But even as definitive as it is, the sleeve gastrectomy is not always a stand-alone solution. In some cases, it is only a stage on the way to more extreme alterations. Cheryl Ann Borne of MyBariatricLife.org says:
Gastric sleeve also can be used as the first step procedure in cases where gastric bypass or duodenal switch are too risky before a significant amount of weight loss, such as in patients with an initial BMI of 50+. In this case, the second bariatric surgery — gastric bypass or duodenal switch — is done somewhere between 6 to 18 months after the gastric sleeve.
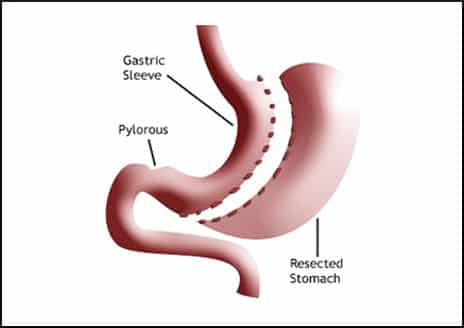
Although the intestine is left untouched, all but about 15% of the stomach is actually removed, so the remaining part is like a tube or sleeve. Amazingly, this can be accomplished with a laparoscopic or so-called “keyhole” approach. However, that does not necessarily mean it is an outpatient procedure. A night or two of hospitalization might follow.
Life After Gastric Sleeve Surgery
The aftermath of a gastric sleeve procedure includes a week of liquid diet and two weeks of pureed food. Solid food can be eaten after that, but the stapled-together stomach incision will not heal for six weeks. Patients who smoke must quit for a month before, and at least a month after, the surgery.
Since the gastric sleeve is a relatively new variation on bariatric surgery, there isn’t a lot of backup data. But from what can be known at present, it appears that 30% to 50% of the excess body weight is shed in the first year, and in the single 6-year followup study, people kept 50% of their excess weight off. As with other procedures, it is possible to “eat through” the remodeled stomach. Overeating can stretch it out and undo the good that was accomplished.
How Popular Is Gastric Sleeve Surgery?
Less than two years ago, at the 24th European Childhood Obesity Group Congress, Dr. Pretlow learned this about the state of the art in bariatric surgery:
Bariatric surgery was claimed to be the treatment of choice for moderate to severe obesity in adolescents. Currently for adolescents bariatric procedures are 28% lapband, 29% sleeve gastrectomy, 18% RNY-bypass, and 18% other. Lapbanding in adolescents has a 25% failure rate pretty much fixed, and 40-50% of the lapbands need to be removed within 5-10 years.
An article published earlier this month describes how the popularity of gastric sleeve surgery has “skyrocketed”:
In the United States, it now makes up over 60% of all weight loss surgery procedures performed, up from 24% in late 2011…The overall short-term risk of gastric sleeve is similar to that of gastric bypass, higher than lap band and lower than duodenal switch. The overall long-term risk of gastric sleeve is lower than all other procedures.
Five years ago, disillusioned blogger Sue Joan characterized the sleeve gastrectomy’s claim to be less invasive as “so not true,” and said this is not widely known because nobody wants to admit that they made an expensive and irreparable mistake. She wrote:
Some of us call this the “conspiracy of silence,” the lack of negative information about weight loss surgery which leads 200,000 people a year to get cut without really knowing what the repercussions might be.
She mentioned an aspect that has not changed—the patient’s difficulty with eating bulky yet healthful foods like vegetables. In her view, it is all too easy for a person to give in to the impulse to favor soft and easily assimilated foods like ice cream and milkshakes. But the technology behind home juicing machines has improved since then, so maybe following a good diet is easier now. At any rate, Sue Joan quoted weight loss surgeon Terry Simpson, MD:
Success with weight loss surgery is 10 percent the surgery, 90 percent the patient.
Your responses and feedback are welcome!
Source: “Gastric Sleeve Surgery Facts,” MyBariatricLife.org, undated
Source: “Gastric Sleeve Surgery: Complete Patient Guide,” Bariatric-Surgery-Source.com, November 2015
Source: “Suethsayings.” blogspot.com, 05/25/10
Image by Veterans Administration

 FAQs and Media Requests:
FAQs and Media Requests: 











