Many medical professionals hold that leaky gut syndrome is indeed a thing. For instance, Dr. Noel T. Mueller says:
It is believed that increased gut permeability can lead to immune-mediated inflammatory cascades that ultimately result in obesity and other metabolic diseases.
When items penetrate the gut wall that aren’t meant to, the gut is said to be leaky. Toxins, endotoxins, metabolic waste products, viruses, proteins, bacteria, yeast, food that is partially undigested — these substances are not supposed to be running around loose in the bloodstream, and when they are let through, trouble ensues.
The intestinal lining’s degree of permeability is not always the same but can be affected by what Dr. David. M. Marquis calls “chemically mediated conditions.” The examples he gives are elevated cortisol because of an argument, and fluctuating thyroid hormone levels provoked by staying up late to study for an exam.
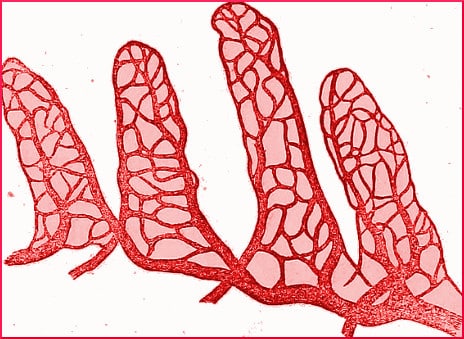
Dr. Marquis explains how the lining of the gut, if spread out flat, could have a surface area equivalent to two tennis courts, every bit of it covered with microvilli. Damaged microvilli can’t do their job, can’t soak up the nutrients and enzymes they are stationed there to capture.
Things that are supposed to get through, can’t. Even worse, junk molecules get through the membrane that aren’t supposed to, and the body identifies them as enemies, and sets up a defense.
Michael Pollan mentions the collaborative process with the microbiome. While most of the body’s tissues get their nutrition from the bloodstream, the colon’s epithelial cells get theirs from short-chain fatty acids made on the spot by gut bacteria. If that epithelial barrier doesn’t receive its preferred nourishment, it becomes more permeable.
Apparently, quite a few adverse conditions can increase the permeability of the barrier. One appears to be the selfish burrowing activities of the bacterium H. pylori.
Others are said to be parasites and a high-sugar diet. Still others, listed by ScientificAmerican.com, include:
Regular use of painkillers, regular use of antibiotics, infections (such as HIV), autoimmune disorders, alcohol abuse, inflammatory bowel disease, gluten hypersensitivity, severe food allergies, radiation therapy, inflammatory disorders, psychological stress, exhaustion.
On the outside of our bodies, the skin has seven layers. In contrast, the epithelium inside the gastrointestinal tract is only one layer thick, so nutrients can pass through it into the bloodstream. Only food that has been completely broken down is welcome, and that is the problem.
The word “barrier” is used, but it is misleading, because the epithelium is so thin, it doesn’t present much of a challenge to aggressive particles that also want to penetrate it. There are big spaces between its cells.
When a condition of “increased GI permeability” exists, and molecules get through that don’t belong, the immune system identifies them as foreign, and calls on its resources to attack the invader. The resulting dysfunctions can adversely affect the tight junctions even more.
When auto-immunity kicks in, all hell breaks loose. The auto-immune responses and resulting inflammation can set off an internal chain reaction that includes depression and fatigue. A tired, depressed person does not have the initiative to cook a healthful meal from fresh foods. A tired, depressed person sits down with a few beers and a bag of chips, and the cycle of destruction continues.
Your responses and feedback are welcome!
Source: “The Gut Microbiome and Childhood Obesity: Connecting the Dots,” mchtraining.net, June 2015
Source: “How Inflammation Affects Every Aspect of Your Health,” Reset.me, 12/08/16
Source: “Some of My Best Friends Are Germs,” MichaelPollan.com, 05/15/13
Source: “Gut Bacteria May Exacerbate Depression,” ScientificAmerican.com, 11/01/13
Source: “Episode 31 with Mike Mutzel,” SigmaNiutrotopm/com, 2014
Photo credit: Internet Archive Book Images via Visualhunt/No known copyright restrictions

 FAQs and Media Requests:
FAQs and Media Requests: 











